The Power of Exercise in Diabetes Management: A Comprehensive Guide
Living with diabetes can feel like a constant balancing act, but what if you had a powerful ally right at your fingertips? Enter exercise - your secret weapon for taking charge of your health. Imagine transforming your daily movement into a strategy that helps keep your blood sugar in check and boosts your overall well-being.
Understanding the Benefits of Regular Exercise for Diabetes
Physical activity is more than just a fitness routine - it’s a critical tool in managing diabetes. Here’s how exercise makes a difference:
Blood Sugar Control
Exercise works like a natural medicine for diabetes management. When you move your body, muscles use glucose more effectively, improving insulin sensitivity. This means:
Your body becomes more efficient at processing sugar
Blood glucose levels become more stable
You reduce the risk of blood sugar spikes and crashes
Weight-loss and Type 2 Diabetes
For individuals with Type 2 Diabetes, exercise offers a unique opportunity to address weight management - a critical factor in disease progression. Research has shown that losing just 5-10% of body weight can significantly improve clinical outcomes such as Hemoglobin A1C, blood pressure, and cholesterol levels, potentially reducing or even reversing type 2 diabetes symptoms (Wing et al., 2011). For example, a person weighing 300 lbs would need to lose 15-30 lbs to lose 5-10% of their body weight (300x5% = 15, 300x10%=30). Regular physical activity helps burn calories, build lean muscle mass, and boost metabolism, creating a powerful combination for weight loss and blood sugar control.
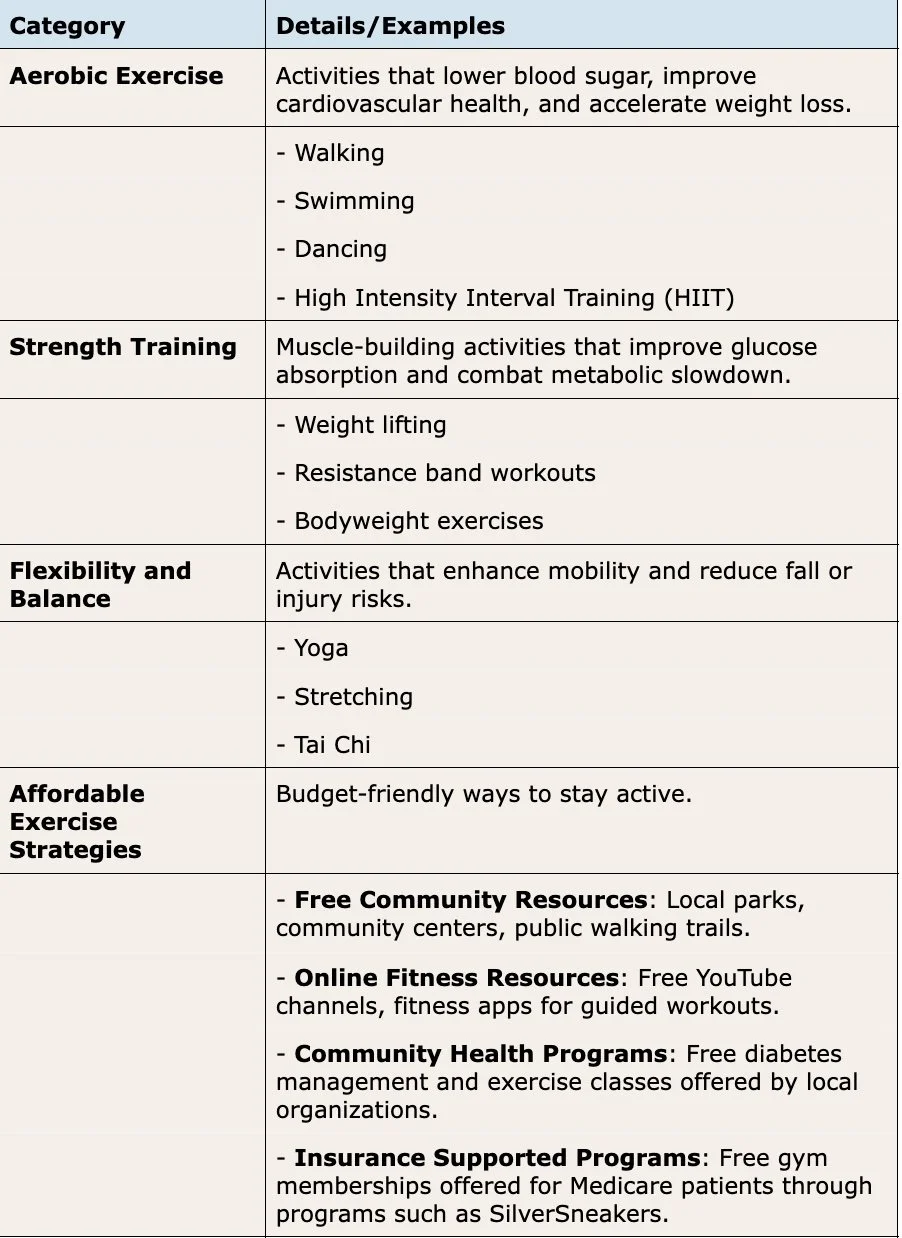
Types of Beneficial Exercises
Not all exercises are created equal when it comes to diabetes management. Here are some standout options:
Creating a Personalized Exercise Plan
Step-by-Step Guide
Consult Your Healthcare Provider: Before starting any new exercise regimen, it’s important to get medical clearance from your healthcare provider. This involves a discussion about your current health status, potential exercise limitations, and developing a safe, realistic, and personalized approach that aligns with your specific medical needs and diabetes management goals.
Talk With a Personal Trainer: If you’re unable to see your healthcare provider in the near future, consulting a personal trainer can be a helpful alternative. Personal trainers can recommend exercises tailored to your needs, demonstrate how to perform them safely, and provide guidance to ensure you're on track toward your fitness goals.
Set Realistic Goals: The key to sustainable exercise is starting small and gradually increasing intensity. Choose activities that you genuinely enjoy, as this will make your fitness journey more enjoyable and likely to become a long-term habit. Remember, the goal is consistency over perfection. Your approach should be gentle and progressive, allowing your body to adapt and your confidence to build naturally.
Track Your Progress: Monitoring your fitness journey can be a helpful tool for staying motivated and understanding your body’s response to exercise. Utilize a fitness tracker app or a journal to log your activities, and pay special attention to tracking your blood sugar levels before and after exercise. This not only helps you understand how different activities impact your glucose levels but also provides an opportunity to celebrate small victories along the way, reinforcing your commitment to health and wellness.
Overcoming Exercise Barriers
Conquering the challenges of maintaining an exercise routine requires strategy and self-compassion. Treat your workouts like important appointments, block out time in your calendar, and prioritize your fitness commitment. Working out around the same time each day may be helpful in staying consistent. Consider finding an exercise buddy who can provide motivation, accountability, and make your fitness journey more enjoyable. Be flexible with your approach, choosing activities that seamlessly integrate into your lifestyle rather than feeling like a burdensome chore.
Most importantly, practice self-kindness. If you miss a workout, don’t view it as a failure but as a normal part of any health journey. The key is consistency over perfection and being gentle with yourself while maintaining forward momentum.
Safety First: Exercise Precautions for Diabetes Management
Blood Sugar Monitoring: Monitoring blood sugar is a critical aspect of safe exercise for individuals with diabetes because specific exercises or intensities of exercise may cause blood sugar to drop to unsafe levels. Before starting any physical activity, be sure to check your glucose levels to ensure they’re within a safe range. Always keep fast-acting carbohydrates nearby in case of unexpected blood sugar drops, and take the time to learn and recognize the signs of low blood sugar. Being prepared and attentive can help you respond quickly to any potential glucose fluctuations during exercise.
Preventing Exercise-Related Complications: Preventing complications requires a proactive and mindful approach. Staying well-hydrated is crucial, as proper fluid intake helps regulate your body’s systems during physical activity. Invest in proper footwear that provides support and reduces the risk of injury, which is particularly important for those with diabetes who may have reduced sensation in their feet. Most importantly, listen to your body - if you feel unwell, dizzy, or experience any unusual symptoms, stop exercising immediately and assess your condition.
Conclusion
Think of exercise as more than just a workout. It's a personalized health toolkit that can adapt to your life, whether you're more into lifting weights, finding zen in yoga, or enjoying a brisk walk. Each step, stretch, and rep is a small victory in managing your diabetes.
The magic of physical activity goes beyond burning calories. It's about increasing your body's insulin sensitivity, reducing the risk of diabetes-related complications, and giving you a sense of control. No matter your fitness level or lifestyle, there's an exercise approach that can work for you.
This guide isn't about creating a one-size-fits-all plan. It's about empowering you to discover movement that feels good, keeps you safe, and supports your health journey. Ready to turn exercise into your diabetes management ally? Start today, and remember - every moment of movement is a step towards better health.
*Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider before beginning any new exercise program or making changes to your health regimen.
Reference:
Wing, R. R., Lang, W., Wadden, T. A., Safford, M., Knowler, W. C., Bertoni, A. G., Hill, J. O., Brancati, F. L., Peters, A., Wagenknecht, L., & Look AHEAD Research Group (2011). Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes care, 34(7), 1481–1486. https://doi.org/10.2337/dc10-2415